#SARS-CoV-2 goes ‘underground’ to spread from cell to cell

“#SARS-CoV-2 goes ‘underground’ to spread from cell to cell”
The virus that causes COVID-19 has adopted some stealth moves to stay alive and kicking, and one secret to its success is hiding from the immune system by spreading through cell-to-cell transmission, a new study has found.
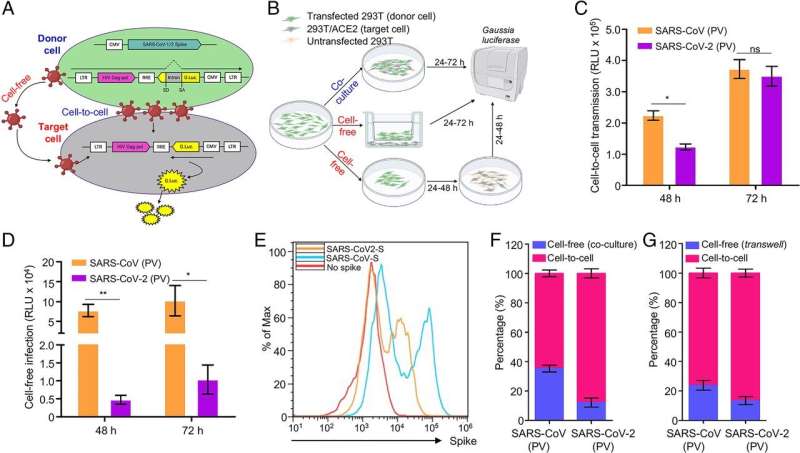
Cell culture experiments showed that SARS-CoV-2, which causes COVID-19, limits the release of viral particles that can be inactivated by antibodies, instead staying tucked within cell walls and spreading between cells.
“It’s basically an underground form of transmission,” said lead author Shan-Lu Liu, a virology professor in the Department of Veterinary Biosciences at The Ohio State University and an investigator in the university’s Center for Retrovirus Research.
“SARS-CoV-2 can spread efficiently from cell to cell because there are essentially no blockers from the host immunity. Target cells become donor cells, and it just becomes a wave of spread, as the virus may not get out of the cells.”
Liu and colleagues found other revealing details about SARS-CoV-2: The spike protein on its surface alone enables cell-to-cell transmission, and yet the virus’s primary receptor on target cells—to which the spike binds—is not a necessary part of the cell-to-cell transmission operation. Additionally, they found that neutralizing antibodies are less effective against the virus when it spreads through cells.
The research was published Dec. 22, 2021, in the journal Proceedings of the National Academy of Sciences.
A major point of this study was comparing SARS-CoV-2 to the coronavirus behind the 2003 SARS outbreak, known as SARS-CoV. The findings help explain why while the first outbreak led to much higher fatality rates and lasted only eight months, we’re about to surpass the two-year mark of the current pandemic, with a majority of cases being asymptomatic, Liu said.
The comparison showed that the SARS-CoV that caused SARS in 2003 is more efficient than SARS-CoV-2 at what is called cell-free transmission, when freely floating viral particles infect target cells by binding to a receptor on their surface—but also remain vulnerable to antibodies produced by previous infection and vaccines. SARS-CoV-2, on the other hand, is more efficient at cell-to-cell transmission—which makes it harder to neutralize with antibodies.
The viruses’ differing efficiencies were first demonstrated in experiments using pseudoviruses—a non-infectious viral core decorated with both kinds of coronavirus spike proteins on the surface.
“The spike protein is necessary and sufficient for both SARS-CoV-2 and SARS-CoV cell-to-cell transmission because the only difference in these pseudoviruses were the spike proteins,” said Liu, also a program director of the Viruses and Emerging Pathogens Program in Ohio State’s Infectious Diseases Institute.
Looking more deeply into those differences, the researchers found that SARS-CoV-2 is also more capable than SARS-CoV at initiating fusion with a target cell membrane, another key step in the viral entry process. And that stronger fusion action was associated with the virus’s enhanced cell-to-cell transmission.
Paradoxically, too much cell membrane fusion leads to cell death and can actually interfere with cell-to-cell transmission, Liu also found.
The team then turned to the role of the ACE2 receptor, a protein on cell surfaces that acts as the gateway for entry of the virus that causes COVID-19. The researchers found, unexpectedly, that cells with no or low levels of ACE2 on their surfaces can be penetrated by the virus, enabling robust cell-to-cell transmission.
“There is no perfect correlation between SARS-CoV-2 infection and the level of ACE2,” Liu said. “ACE2 may be needed for initial infection, but once infection is established, the virus may not need ACE2 anymore because it can spread from cell to cell.”
Finally, in experiments testing blood samples from human COVID-19 patients against the authentic SARS-CoV-2 virus, researchers determined that the virus could evade an antibody response through cell-to-cell transmission, but that antibody neutralization of the virus in the cell-free transmission mode was effective.
“We were able to confirm cell-to-cell transmission is not sensitive to inhibition from antibodies from COVID patients or vaccinated individuals,” Liu said. “Cell-to-cell transmission’s resistance to antibody neutralization is probably something we should watch for as SARS-CoV-2 variants continue to emerge, including the most recent, Omicron. In this sense, developing effective antiviral drugs targeting other steps of viral infection is critical.”
There are still many unknowns, including the exact mechanism the virus uses to spread from cell to cell, how that may influence individuals’ responses to viral infection, and whether or not efficient cell-to-cell transmission contributes to the emergence and spread of new variants. Liu’s lab is planning additional studies using the authentic virus and human lung cells to further explore these questions.
Cong Zeng et al, SARS-CoV-2 spreads through cell-to-cell transmission, Proceedings of the National Academy of Sciences (2021). DOI: 10.1073/pnas.2111400119
Citation:
SARS-CoV-2 goes ‘underground’ to spread from cell to cell (2021, December 23)
retrieved 23 December 2021
from https://phys.org/news/2021-12-sars-cov-underground-cell.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.
If you liked the article, do not forget to share it with your friends. Follow us on Google News too, click on the star and choose us from your favorites.
For forums sites go to Forum.BuradaBiliyorum.Com
If you want to read more Like this articles, you can visit our Science category.




